Researchers at the University of Nebraska–Lincoln are working to halt resistance to an antibiotic that treats serious staph infections in humans.
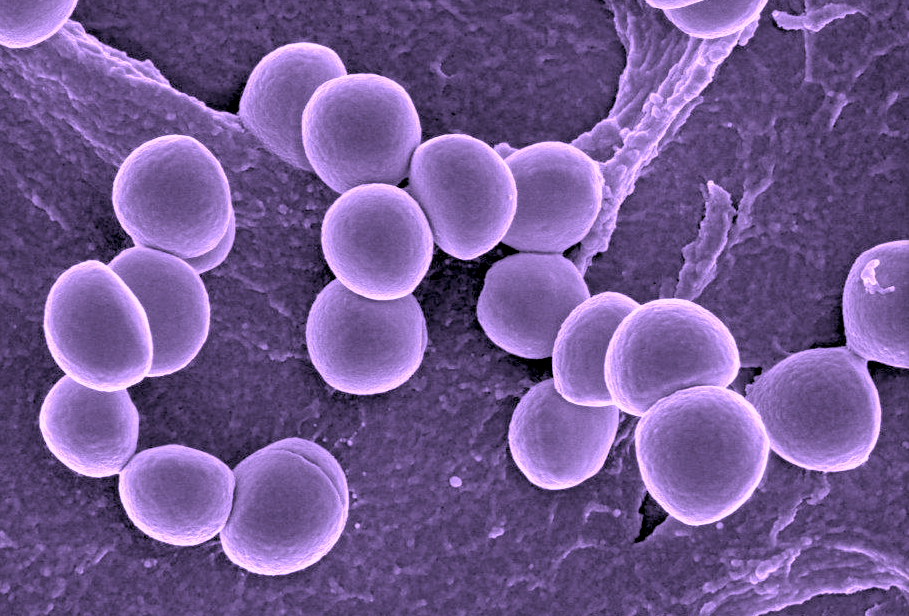
Staphylococcus aureus is a bacterium commonly found on the skin or noses of people and animals, even healthy ones. While this bacterium is a common cause of skin infections, it can invade other areas of the body and cause life-threatening infections. In fact, the bacterium causes more deaths in the United States than does HIV/AIDS.
“Staphylococcus aureus is one of the more versatile bacteria out there,” said Greg Somerville, associate professor of veterinary medicine and biomedical sciences. “In dairy animals, this bacterium can cause mastitis, an economically and medically important infectious disease in Nebraska and worldwide.”
A growing challenge in the treatment of staph infections is that the bacteria can become resistant to antibiotics, including daptomycin. Antibiotic resistance not only complicates the treatment of many infections, it also raises the cost of treating those infections. A recent United Nations report claims that drug-resistant diseases could kill 10 million people a year by 2050.
Somerville and his colleagues have conducted research on the metabolic changes that occur in the bacteria before and after the development of resistance. This information was used to develop a new treatment plan that uses daptomycin in combination with another drug already approved for use in humans. The advantage to finding a combination involving daptomycin is that it provides a solution without waiting for a new antibiotic to receive approval from the U.S. Food and Drug Administration, which can take several years and be very costly. A recent study estimated that developing a new prescription medication can cost pharmaceutical companies $2.6 billion.
“Our research found that the metabolic adaptations associated with staph resistance can be targeted to prevent the emergence of resistance to daptomycin,” Somerville said. “In addition, you can target metabolism to overcome existing resistance.”
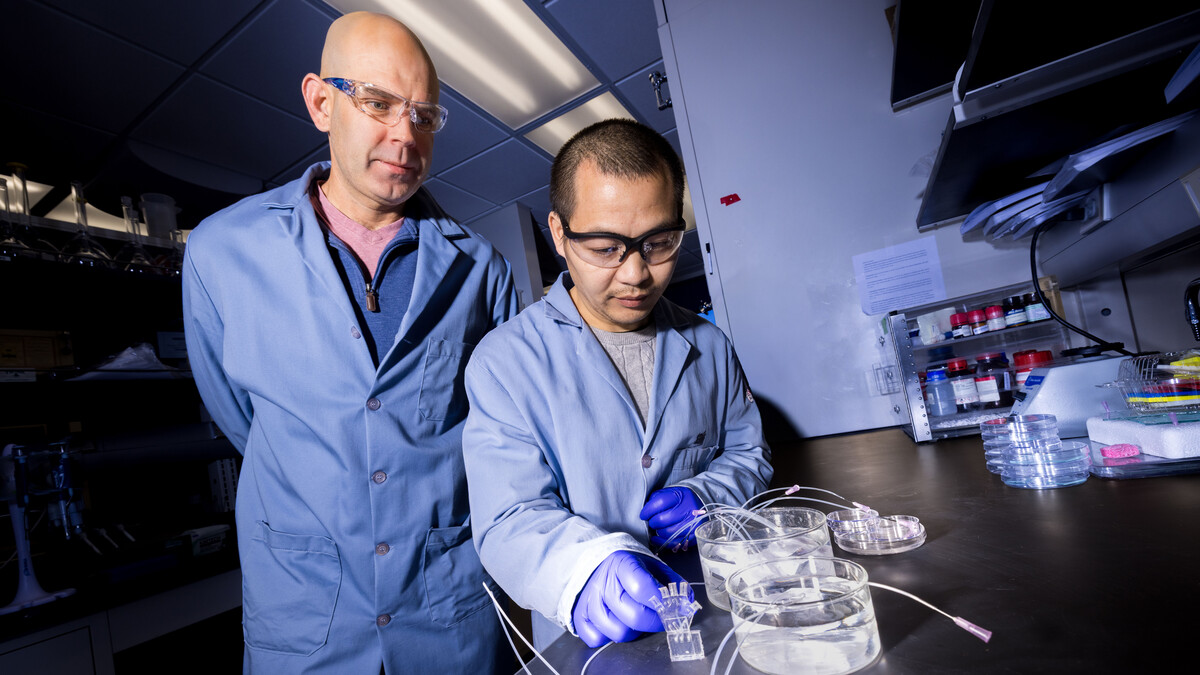
Somerville attributed the advancement of this research to key collaborations across disciplines. One of those collaborations is with Robert Powers, professor of chemistry. The two have collaborated for over a decade and said that the complementary nature of their expertise facilitated this project and others.
“This research demonstrates the value of leveraging the metabolome to understand fundamental processes in cellular biology that can be used as a valuable resource in drug discovery and disease diagnostics,” Powers said.
Others involved with this research include Stewart Gardner, postdoctoral fellow, and Joseph Reed, graduate student, in the School of Veterinary Medicine and Biomedical Sciences; along with Arnold Bayer, distinguished professor of medicine, and Nagendra Mishra, assistant professor, at the David Geffen School of Medicine at the University of California, Los Angeles.
A summary of the team’s findings was recently published in the Journal of Antimicrobial Chemotherapy.